A recent study revealed promising findings regarding a novel schizophrenia medication, Cobenfy, which many participants showed improvement while experiencing only a few side effects. However, a significant number of individuals decided to withdraw from the trial, highlighting the ongoing challenges associated with treating schizophrenia, a complex mental health condition marked by symptoms such as auditory hallucinations, paranoia, and social withdrawal. These high dropout rates are seen frequently in studies focused on schizophrenia therapies.
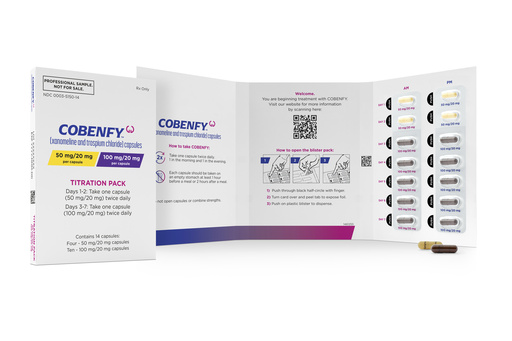
The quest for effective treatment can often feel prolonged, sometimes accompanied by significant crises and hospital visits. Many existing medications pose side effects such as weight gain, tremors, and restlessness that lead some patients to cease their treatment, resulting in relapses. Cobenfy, which received FDA approval in September, has generated considerable hope among healthcare professionals because of its unique mechanism of action. Unlike traditional drugs that target dopamine receptors, Cobenfy’s primary component, xanomeline, interacts with different receptors to indirectly inhibit dopamine release.
Additionally, Cobenfy includes trospium, which targets some common side effects experienced with antipsychotic treatments. While nausea, vomiting, and digestive issues remain the typical side effects, the medication has been noted for helping users shed a few pounds, a benefit unlike other schizophrenia medications, often associated with weight gain. Bristol Myers Squibb, the company behind Cobenfy, seeks to provide a better treatment option for those affected by schizophrenia.
Dr. John Krystal of Yale, an expert who has researched various schizophrenia treatments, acknowledged that only 10% to 20% of participants withdrew from the latest trials due to side effects—a noticeable improvement. He emphasized the potential benefits of fewer side effects, which might encourage individuals to maintain their treatment regimen, ultimately reducing complications related to untreated mental disorders such as substance abuse, homelessness, and job loss.
Understanding the disparity between participants who continued their treatment and those who left is crucial as healthcare professionals begin to prescribe Cobenfy. The FDA granted approval primarily based on two encouraging short-term studies. However, the recent results presented at the Psych Congress meeting in Boston stem from two extended trials, offering a deeper insight into the drug’s effectiveness.
In one trial with severely ill patients, 78% discontinued their participation, which left only 35 individuals for final analysis. Conversely, in the second group, comprised of more stable patients, 51% dropped out, resulting in 283 participants who remained on the medication for a year. Dr. Greg Mattingly of Washington University stated that these dropout rates are comparable to typical figures seen in studies concerning schizophrenia.
Among the severely ill participants, 69% reported significant symptom relief by the end of the year, while 30% of the more stable group also observed meaningful benefits. An evaluation by an independent research team highlighted that, six months post-trial, 36 participants expressed interest in continuing treatment with Cobenfy, while only 10 stated they would prefer not to. Experiences varied, with some individuals reporting a decrease in hallucinations and others feeling the medication was ineffective.
The anticipated annual cost of Cobenfy is $22,500, a stark contrast to the $540 for generic versions of antipsychotic medications. Experts are concerned that insurance providers may mandate trying less expensive alternatives prior to approving coverage for Cobenfy. One such alternative, clozapine, is a well-regarded treatment option for schizophrenia but is not frequently utilized in the U.S. due to a demanding blood monitoring protocol established amidst concerns about severe neutropenia, a rare but potentially fatal side effect.
Individuals and families have reported that the blood tests have sometimes delayed or interrupted critical treatment, resulting in relapses due to withheld clozapine. Testimonials from patients like Sally Littlefield, who relies on long-acting antipsychotic injections, reflect a desire for more diverse perspectives on Cobenfy beyond those closely tied to its development.
Similarly, Mindy Greiling is curious about how Cobenfy stacks up against clozapine, which has effectively managed her son Jim’s condition. Although he faced weight gain challenges, his current diabetes medication has helped normalize his weight. She expressed skepticism regarding Cobenfy’s hype, indicating it would need to demonstrate superior benefits compared to clozapine to be considered a viable option.
