In a recent breakthrough, researchers have gained valuable insights into how the human brain eliminates waste, an important factor in the development of Alzheimer’s disease. The brain, known for its extensive use of nutrients, generates considerable waste, and scientists have long speculated about a distinct system that helps to clear this debris, especially during sleep—an effect previously observed in mice. However, direct evidence of a similar mechanism in humans had been lacking until now.
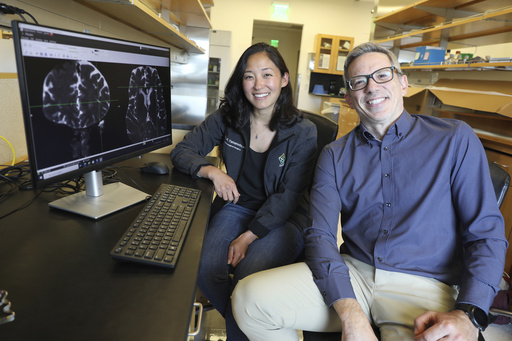
Researchers have now identified a network of tiny channels within the brain that facilitate this waste removal, thanks to advanced imaging techniques. Dr. Juan Piantino of Oregon Health & Science University, one of the study’s contributors, expressed his initial skepticism regarding the existence of this system in humans, stating the necessity for concrete evidence to validate its occurrence.
Published in the Proceedings of the National Academy of Sciences, the study highlights the brain’s significant activity during sleep, which appears to be integral to its cleansing operations. This is particularly relevant considering that sleep deprivation can impair cognitive functions and has been linked to an increased risk of dementia.
The concept of a cleansing system in the brain, referred to as the “glymphatic system,” was first introduced over ten years ago by researchers at the University of Rochester. Their findings indicated that cerebrospinal fluid travels through channels surrounding blood vessels to effectively push waste out of the brain. Experimentation in mice revealed that substances like beta-amyloid—known to contribute to Alzheimer’s disease—were cleared more efficiently during sleep.
Despite this understanding, confirming the presence and functionality of the glymphatic system in humans posed challenges. While traditional MRI scans can reveal the location of fluid-filled channels, they do not provide information on their operational dynamics. To overcome this limitation, Piantino’s team employed a tracer injected into five patients undergoing brain surgery, which was then tracked using a more sophisticated form of MRI. The results showed that, akin to previous results in mice, the tracer flowed along specific channels within the brain rather than dispersing randomly.
This initial study, though small, has the potential to spark greater interest in the relationship between brain waste clearance and overall health, as noted by Dr. Maiken Nedergaard from Rochester. However, Dr. Jeff Iliff of the University of Washington emphasized the need to develop methods for measuring glymphatic function in humans to explore whether improved sleep or other treatments could enhance waste clearance and promote better health outcomes. The findings may inspire new measurements and investigations into this critical area of research.
Additionally, sleep isn’t the only factor under consideration. Preliminary studies on animals suggest that certain medications, including an existing blood pressure drug used for PTSD treatment, may enhance glymphatic function. Both Iliff and Dr. Elaine Peskind are poised to investigate this possibility in specific patient groups. More extensive studies involving healthy individuals are essential, and Piantino’s team is eager to create a more straightforward and non-invasive assessment method.
As the possibilities for studying brain health evolve, researchers remain optimistic about uncovering how sleep and other interventions could influence this vital waste clearance mechanism. Without techniques that require invasive procedures, there exists a broad spectrum of questions waiting to be explored.