A new study documents lost opportunities to treat drug overdose survivors covered by the Medicare program — and illustrates the difficulty of managing chronic pain.
Overdose survivors “should be at the front of the line for the full range of medications and counseling and support,” said Dr. Brian Hurley, president of the American Society of Addiction Medicine, who was not involved in the study, published Monday in JAMA Internal Medicine.
Instead, those on Medicare who survived a drug overdose in 2020 were much more likely to later receive opioid painkillers than any medication to treat addiction — and some went on to die of an overdose.
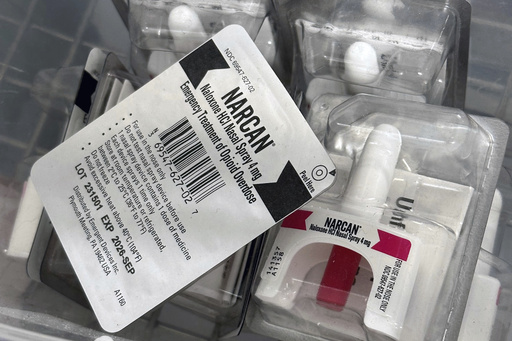
U.S. government researchers found 53% of overdose survivors received opioid painkillers while 4% received treatments such as buprenorphine. Only 6% filled prescriptions for the overdose antidote naloxone. Within a year of their overdose, 17% experienced a second nonfatal overdose and 1% died of an overdose.
The researchers looked at nearly 137,000 Medicare beneficiaries who survived an overdose in 2020, when the emergence of COVID-19 scrambled drug treatment efforts.
The group included about 30% who qualified for Medicare because of a disability rather than their age. About 80% of them had been treated for acute or chronic pain, and nearly half had prescriptions for opioids before the overdose.
In some situations, it might be appropriate to continue to prescribe opioids after an overdose, but “these patients should be closely monitored, provided naloxone” and have plans in place to reduce overdose risk, said lead author Capt. Christopher Jones of the Substance Abuse and Mental Health Services Administration.
Gaps in treatment for overdose survivors exist throughout the U.S. health care system and predate the pandemic, said Dr. Michael Barnett of the Harvard T.H. Chan School of Public Health, who was not involved in the new study, but found similar results among Medicare patients from 2016-2019.
“The health system is very poor at connecting people to life-saving medication after they overdose,” Barnett said. “It’s a health system problem. And it’s also a problem of stigma and public education that many people may not be interested or may not trust medications for opioid use disorder.”
In 2020, Medicare expanded coverage to include methadone to address a longstanding treatment gap. Methadone is the oldest, and experts say, the most effective of the three approved medications used to treat opioid addiction. It eases cravings without an intense high, allowing patients to rebuild their lives.
Medicare still does not cover residential addiction treatment, another gap that should be closed, Hurley said.
___
The Associated Press Health and Science Department receives support from the Howard Hughes Medical Institute’s Science and Educational Media Group. The AP is solely responsible for all content.